
We hear about the addictive dangers of opioids all the time–on the news, from doctors, and from family members. But it can be a bit confusing to tell the difference between natural opiates and how they’re different from opioids, as well as opiate treatment and opiate detox.
We break down these terms and discuss the differences between opiate withdrawal and opiate withdrawal symptoms, including an opiate withdrawal timeline and the importance of medical detox. If you or someone you know needs assistance in managing an opioid use disorder, info about finding opiate drug detox centers near you is offered, along with convenient links.
What are Opiates?
Opiates are drugs produced from the opium poppy plant. When they enter the body, opiates bind to opioid receptors in the central nervous system and produce an analgesic, or pain-relieving, effect. Types of naturally occurring opiates include codeine and morphine, which are prescription drugs used to treat pain or induce sleep.
Other opiate-like drugs are derived from natural opium or chemically created in laboratories. Synthetic opium-like drugs that contain natural or chemically modified natural opiate ingredients include heroin and oxycodone. Heroin is derived from morphine, a natural opiate. Oxycodone is chemically derived from another substance found in opium called thebaine.
Other laboratory made drugs, such as fentanyl and methadone, are purely synthetic and entirely created by combining chemicals in the lab. A few synthetic opioid drugs like fentanyl, methadone and buprenorphine are approved for medical use when prescribed by doctors. Other synthetic opioids such as so-called “street drugs” are unregulated and are illegal to use.
Opioids vs. Opiates
Opioids is an umbrella term for both natural opiates and synthetic opiate-like substances. The term opiate refers only to the natural plant-derived compounds. However, both terms–opiates and opioids–are often used interchangeably. The use of either opiates or opioids can lead to addiction.
Common Types of Opiates
- Actiq is also called fentanyl citrate and is a synthetic opioid agonist to treat severe pain. It’s often prescribed for people with chronic conditions, such as cancer, who haven’t responded sufficiently to other opioids. Actiq works by binding to opioid receptors in the central nervous system to block pain signals.
- Demerol is also called meperidine hydrochloride. This drug soothes moderate to severe pain. It’s also a synthetic opioid agonist that binds to opioid receptors in the central nervous system and blocks pain signals.
- Dihydrocodeine is an opioidprescription drug used in place of or alongside codeine totreat moderate to severe pain. It’s a DEA Schedule II controlled substance with a high potential for abuse.
- Dilaudid is the brand name of hydromorphone. This is another prescription opioid that blocks pain signals in the brain. It’s also a Schedule II drug.
- Duragesic is the brand name of a strong fentanyl that’s delivered through a skin patch. It treats acute pain when other pain medications aren’t effective.
- Fentanyl is a synthetic opioid that provides analgesic effects similar to morphine. It’s 100 times stronger than morphine. Fentanyl is approved by the FDA for pain relief and anesthetic use. Fentanyl is also produced illicitly as an illegal and popular street drug.
- Heroin is afast-acting opiate processed from morphine. It’s highly addictive. Heroin is a Schedule I controlled substance with a high potential for abuse and has no accepted medical use.
- Kadian is the brand name of an extended-release morphine sulfate capsule. It is used to treat moderate or severe pain. It’s a Schedule II controlled drug.
- Morphine is a natural opiate derived from opium. It’s made into pharmaceutical products to treat pain. They’re a Schedule II narcotic medication.
- Opana is the brand name for oxymorphone. This prescription opioid analgesic medication treats severe pain.
- Opium is a natural opiate substance obtained from the poppy plant. It’s used to produce narcotic drugs including morphine, heroin, and codeine. Opium is highly addictive and is a Schedule II drug.
- Oxycodone is a potent prescription opioid analgesic medication for severe pain. It’s a Schedule II drug.
Signs and Symptoms of Opiate Addiction
Opiate addiction starts when a person becomes dependent on a drug for physical and psychological comfort. Tolerance to the drug occurs when you require higher doses to achieve the same effect or you get less benefit from the drug over time. You may also experience withdrawal symptoms if you try to stop.
Psychological dependence means that your thoughts and emotions center around your drug use–when and how to get your next dose. This results in cravings and a compulsion to continue using the substance.
Such experiences may cause you to continue using opiates even though doing so leads to problems in your life. Once this occurs, you’re addicted.
Other examples of opiate addiction symptoms include:
- Unsuccessful attempts to cut down
- Spending a great deal of time and effort obtaining the drug
- Failing at home, work or school responsibilities
- Giving up activities or hobbies because of drug use
- Using opiates in risky or hazardous situations
Dangers of Opiate Addiction
Dependence and addiction to opiates occur easily. People sometimes become physically dependent on opiates after using them for a short time to manage pain following surgery. A 2018 study reported that more than 80% of patients received prescriptions for opioid pain medication following their surgeries.
More than 60% of those who received 90 days of continuous opioid therapy still used opiates a year later.
Withdrawal symptoms can occur after taking opiates daily for as little as two weeks, although it typically takes 90 days or longer. One study revealed that 56.5% of patients who initially used prescription opioids for pain relief continued using them mainly to avoid withdrawal symptoms.
Opiate Withdrawal: What to Expect and Common Symptoms
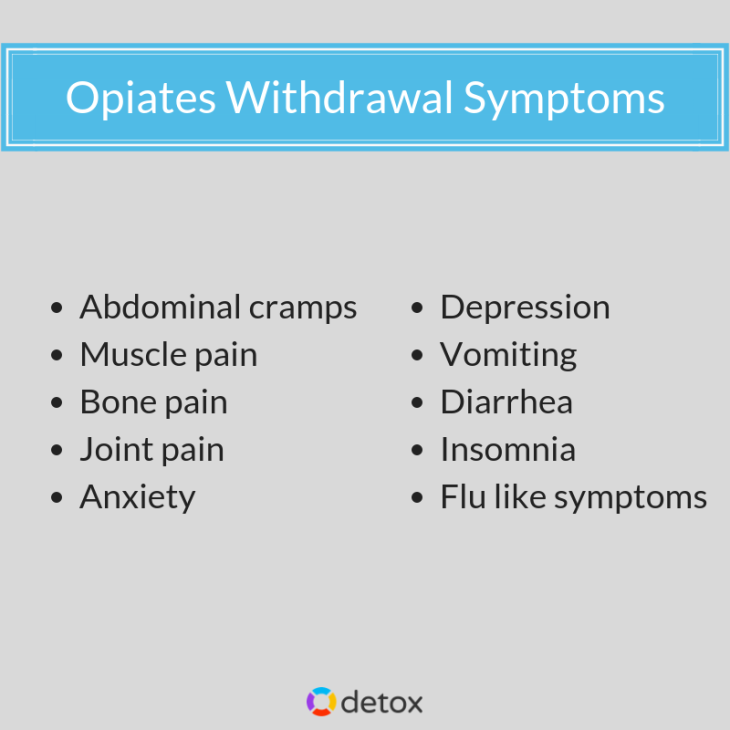
Physical Symptoms may include the following:
- Nausea and vomiting
- Chills
- Fever
- Runny nose
- Diarrhea
- Cramps
- Insomnia
- Heavy sweating
- Elevated heart rate or blood pressure
- Muscle or bone pain
Psychological Symptoms may also occur. You might experience some of the symptoms below:
- Depression
- Anxiety
- Insomnia
- Drug cravings
Other Possible Problems
Mothers who use opiates while pregnant might deliver babies with neonatal abstinence syndrome (NAS). Signs of NAS in newborns include:
- Vomiting
- Fever
- Sweating
- Irritability and difficulty in consoling
- Sleep difficulties, restlessness
- Difficulties sucking or swallowing
- Possible seizures
An Opiate Withdrawal Timeline (Adults)
Here is a brief timeline of a typical withdrawal experience from opioids.
Early symptoms (6-24 hours)
- Anxiety
- Runny nose
- Sweating
Peak Symptoms (1-3 days)
- Vomiting
- Diarrhea
- Insomnia
- Cramps
Subacute Symptoms (4-10 days)
- Depression
- Cravings
- Fatigue
Post-acute Withdrawal Symptoms (PAWS)
- Sleep problems
- Irritability
- Fatigue
- Lack of mental focus
- Anxiety
- Depression
PAWS may be experienced for a few weeks or up to several months as the brain’s chemical balance and neurotransmitters return to normal.
Opiate withdrawal symptoms are difficult to experience. But with determination and treatment, you can break free from your addiction.
Detoxing From Opiates
Since withdrawal from opiates is difficult, you might want to consider detoxification. There are several ways to detox from opiates:
Medical Detox involves receiving 24/7 medical care in a hospital, clinic, or rehab facility as you taper off opiates. Such care is critical for your safety. Medications can help you more comfortably manage withdrawal symptoms. Medications for use in medical detox may include:
- Methadone: binds to the same brain receptors as opiates but activates them more slowly and remains in the body longer. This results in less intense pleasurable feelings being produced so that the patient can wean off their dependency with fewer withdrawal symptoms and drug cravings.
- Buprenorphine (Suboxone) is like methadone and binds to the same brain receptors as opiates. However, it does so to a lesser degree than methadone and it activates opiate receptors with less intensity.
- Clonidine is sometimes used during early opiate detox. Clonidine calms sympathetic nervous system activity. It’s often used during and after tapering off methadone or buprenorphine.
Call now to detox and get clean today.
Rapid Detox takes place in a controlled environment where patients can be closely monitored. Medications are used to reverse the effects of opioids. Sometimes sedation is used to allow the patient to remain comfortable during an accelerated detox that might be completed in a few days instead of a week or two.
While rapid detox is faster, controversy exists about its efficacy and safety when compared to traditional detox methods. For these reasons, some insurances consider rapid detox to be an experimental procedure and don’t cover it.
At Home Detox is possible but has risks. You can slowly wean off opiates and manage symptoms with the help of a doctor who may prescribe medication to assist with symptoms. They may recommend over-the-counter medications, as well. This is most likely to work for those who’ve used opiates for a short time, not months or years.
When detoxing at home, you should plan to go to an emergency room or urgent care if withdrawal symptoms become severe.
Dangers of Opiate Detox Without Help
At home opiate detox or going cold turkey aren’t usually recommended for people who have used opiates for a long time or who have used high doses. There is a greater chance for relapse when you don’t have medical and psychological support from professionals. Other risks include dehydration and mental health crises.
How to Find an Opiates Detox Center Near You
If you decide that going to an opiate detox center is your best option, locate detox drug centers near you by using the Substance Abuse and Mental Health Administration’s (SAMHSA) Opioid Treatment Program Directory. You can also find other rehab treatment directories, such as Detox.com. You can search by state and location or by treatment like detox.
Opiate Detox FAQs
Using professional help that’s available at a detox center gives you the best chance for success.
Home detox is possible, but isn’t recommended.
Methadone, buprenorphine, clonidine, and lofexidine are among the many medication options used in opiate detox.
The time it takes to fully detox depends on the type of opiate used and how long it was used. The acute phase often lasts for 5-10 days. Full detox can take up to several months to complete.
Detox is often the initial phase of rehab. But some people go straight into a counseling rehab program while others attend detox only. The optimal process is to go to a rehab center for detox and then stay there for the follow-up treatment.
Treatment After Detox: Rehab & Recovery
After opiates detox, many people find that follow-up programs are helpful. There are many options for follow-up treatment:
Inpatient Treatment takes place ata facility like a hospital, a clinic, or a freestandingdrug rehab. You stay at the facility 24/7 throughout your treatment. Inpatient rehab programs often run for 28-30 days or 60-90 days.
Residents are monitored and attended to by staff that typically includes medical personnel and mental health counselors. Counseling is provided in group and individual sessions. Family sessions and other types of treatment, such as holistic or recreational therapy, are usually included.
Outpatient Treatment may take place at a rehab facility or a counseling office. These don’t include overnight stays. Instead, you attend treatment during the day and return home at night. Programs may last from a week up to several months.
Offerings can involve partial hospitalization programs (PHPs) that deliver all-day sessions 4-6 days a week for a total of 20+ hours of treatment per week and typically lasting 30-90 days. Intensive outpatient programs (IOP) often provide treatment 2-3 days per week for up to 9-20 treatment hours per week. The recommended minimum duration for IOPs is 90 days.
Psychological and behavioral therapies at inpatient and outpatient facilities include group counseling with individual sessions. Therapies often consist of cognitive behavioral therapy (CBT). Contingency management that uses motivational incentives such as gift cards or other rewards to reinforce therapy goals can also be used.
Dialectical behavioral therapy (DBT) is another approach that emphasizes emotional regulation and managing difficult emotions.
Call now to find inpatient and outpatient opiate detox centers near you!
Long-term Recovery Planning Following Rehab Treatment
After rehab treatment, the goal is to prevent relapse and maintain abstinence from drug use. Rehabs like opiate treatment centers often provide alumni groups where program grads can return for fellowship and support group meetings. These may include 12-step meetings or social gatherings.
Some people choose to stay for a few months or more at a recovery home once they’ve completed drug rehab. Recovery homes are also called sober homes and provide drug-free environments. House rules are monitored by a house manager as well as fellow housemates to promote accountability and to maintain recovery goals. Such environments provide helpful transitions back to independence and healthy living.
Opioid use disorders are difficult to tackle, and recovery is often filled with many challenges. But the endgame of recovery is worth the effort not just for you, but your loved ones who support you throughout. A healthier and happier future awaits!

